When it comes to fertility, most people think about ovulation, egg quality, or sperm health. But there’s another piece of the puzzle that often gets overlooked: the luteal phase. A disruption in this part of the menstrual cycle, known as Luteal Phase Deficiency, can quietly affect the chances of conception and early pregnancy.
If you’ve ever felt confused by medical jargon or overwhelmed while trying to make sense of fertility struggles, you’re not alone. This guide is here to break down what luteal phase deficiency is, why it matters, and how it can impact fertility—in plain, conversational language.
Understanding the Menstrual Cycle
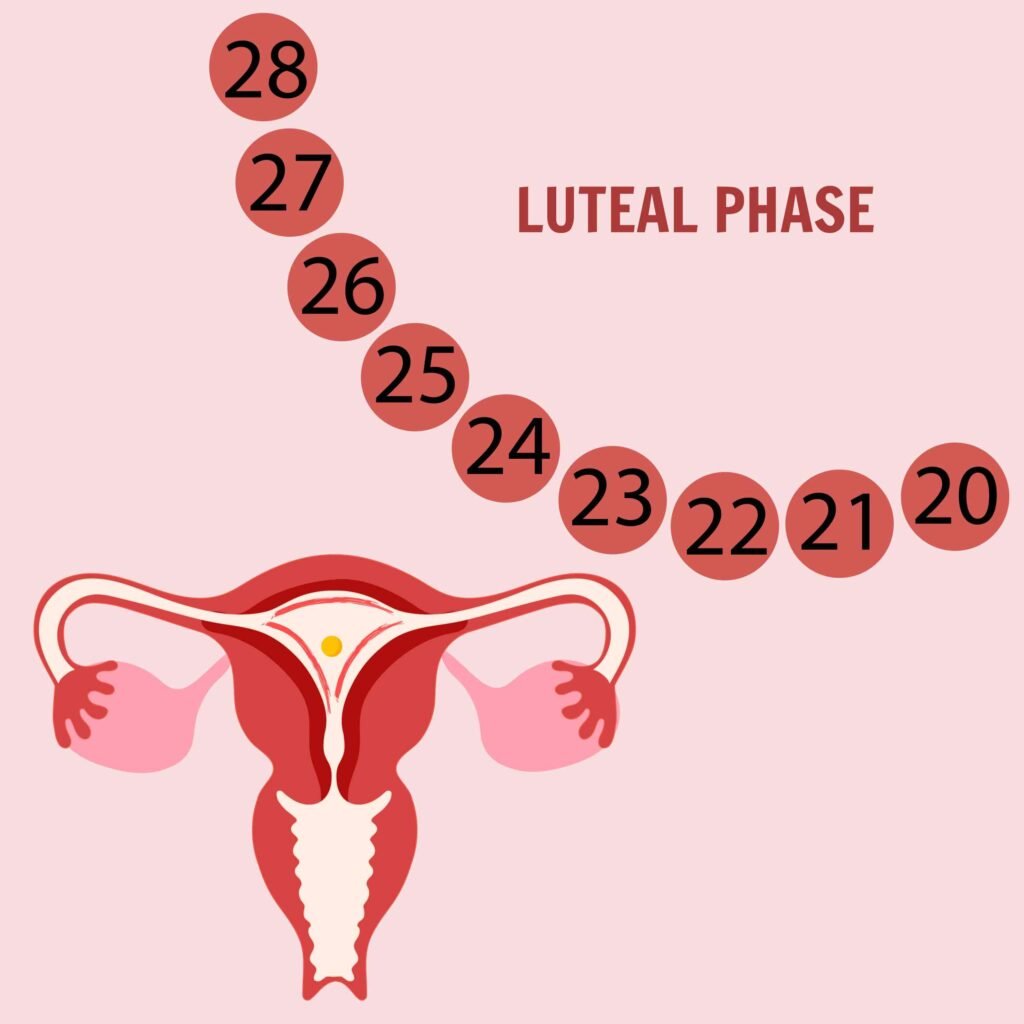
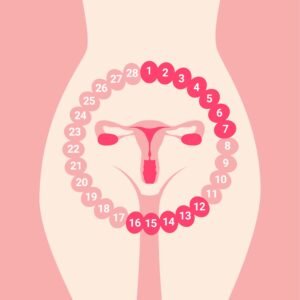
To understand luteal phase issues, we first need to take a closer look at the menstrual cycle itself. The cycle is divided into two main phases:
- Follicular phase –
This begins on the first day of your period and lasts until ovulation. Estrogen is the key hormone here, helping an egg mature and preparing the uterine lining. - Luteal phase –
This comes after ovulation and typically lasts about 12–14 days. Progesterone, produced by the corpus luteum (the temporary structure formed after ovulation), is the star of the show. Its role is to thicken and stabilize the uterine lining so that an embryo can implant and grow.
If the luteal phase is too short or if progesterone levels are insufficient, implantation may fail, or an early pregnancy might not be sustained. That’s where Luteal Phase Deficiency comes into the picture.
What Exactly Is Luteal Phase Deficiency?
Luteal Phase Deficiency (sometimes called luteal phase defect) refers to a condition where the luteal phase of the cycle doesn’t function properly. This could be due to:
- A shortened luteal phase (less than 10 days)
- Low progesterone levels
- Poor response of the uterine lining to progesterone

The result? The endometrium (uterine lining) isn’t adequately prepared to support implantation, and this can contribute to infertility or recurrent early miscarriage.
Think of it like preparing a guest room. If your guests arrive (fertilized egg), but the room hasn’t been cleaned or made ready (uterine lining), it’s tough for them to settle in and stay.
Causes of Luteal Phase Deficiency
There isn’t one single cause—it’s usually a combination of factors. Here are the most common ones:
- Hormonal imbalances: Conditions like polycystic ovary syndrome (PCOS), thyroid disorders, or high prolactin levels can disrupt progesterone production.
- Stress: Chronic stress impacts the hypothalamic-pituitary-ovarian (HPO) axis, which regulates hormones.
- Low body weight or excessive exercise: These can reduce luteinizing hormone (LH) surges and affect ovulation quality.
- Aging: As ovarian reserve declines, so does the quality of ovulation and progesterone production.
- Underlying medical issues: Endometriosis and chronic inflammation in the uterus can interfere with the luteal phase.
Signs and Symptoms
The tricky thing about luteal phase issues is that they often fly under the radar. Still, some subtle clues may suggest a problem:
- Short cycles (less than 24 days)
- Spotting between ovulation and menstruation
- Difficulty conceiving despite timed intercourse
- Repeated early miscarriages
- Premenstrual symptoms that start earlier or feel more intense

Of course, these symptoms don’t always mean you have Luteal Phase Deficiency, but they’re worth noting and discussing with a healthcare professional.
How Luteal Phase Deficiency Is Diagnosed
This is where things get a bit complicated. There’s ongoing debate in the medical world about whether luteal phase defect is a distinct condition or just a symptom of other reproductive problems. Still, doctors use several approaches to investigate:
- Tracking cycle length: A luteal phase shorter than 10 days is a red flag.
- Progesterone blood tests: Taken about 7 days after ovulation, they measure whether progesterone levels are high enough.
- Endometrial biopsy: Though less common now, this involves sampling uterine tissue to see if it matches the expected phase of the cycle.
- Ultrasound monitoring: Can help confirm ovulation and assess follicle development.
Luteal Phase Deficiency and Infertility
Here’s where it all ties together: fertility relies on a delicate dance of hormones and timing. Even if ovulation happens perfectly and sperm meets egg, implantation still requires the uterine lining to be welcoming and ready.
With Luteal Phase Deficiency, that lining may be too thin, unstable, or prematurely breaking down. The consequences include:
- Lower chances of implantation
- Higher risk of chemical pregnancies (very early miscarriages)
- Recurrent pregnancy loss
In some women, luteal phase problems are the main hurdle; in others, they’re just part of a bigger picture of reproductive challenges.
Treatment Options
The good news is that there are ways to support or correct luteal phase function. Treatments are usually personalized based on the underlying cause, but common approaches include:
1. Progesterone Supplementation
This is the most straightforward method. Progesterone can be given orally, vaginally, or via injections after ovulation or embryo transfer (in IVF). It helps stabilize the uterine lining.
2. Ovulation Induction
Medications like clomiphene citrate or letrozole may be prescribed to improve ovulation quality, leading to better corpus luteum function and higher progesterone levels.
3. hCG Injections
Human chorionic gonadotropin can be administered to mimic natural LH, supporting the corpus luteum and boosting progesterone.
4. Addressing Underlying Conditions
- Treating thyroid imbalances or hyperprolactinemia
- Managing PCOS with lifestyle changes or medications
- Reducing inflammation caused by endometriosis
5. Lifestyle Adjustments
Stress management, maintaining a healthy weight, and balanced nutrition can all positively impact hormonal function.

Luteal Phase Deficiency in Assisted Reproductive Technology (ART)
Interestingly, luteal phase support is almost routine in fertility treatments like IVF. That’s because the medications used during stimulation can suppress natural progesterone production. Even women without a known deficiency are often given supplemental progesterone during the luteal phase of IVF cycles to improve implantation rates.
This highlights just how important the luteal phase is for pregnancy success.
Coping With Fertility Struggles
Beyond the medical side, facing infertility can be emotionally taxing. If you’re dealing with suspected luteal phase problems, here are a few supportive steps:
- Seek a second opinion: Reproductive endocrinologists specialize in these nuanced issues.
- Track your cycles carefully: Apps and ovulation kits can help you spot patterns.
- Join support groups: Talking to others who understand can reduce isolation.
- Practice self-compassion: Struggling with fertility is not your fault.
Final Thoughts
Fertility is complex, and there’s rarely a single explanation for difficulties conceiving. Still, understanding and addressing Luteal Phase Deficiency may be the missing piece for some women. If you suspect this might be affecting you, it’s worth talking to a knowledgeable doctor who can explore both medical and lifestyle approaches.
Remember: infertility doesn’t define you, and there are many paths to parenthood. Whether through medical treatments, assisted reproduction, or alternative family-building options, hope is always part of the story.